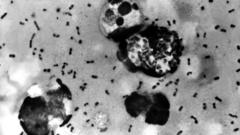
The resurgence of measles in Canada has raised alarm as the country faces an unprecedented number of cases, largely stemming from low vaccination rates and misinformation surrounding immunizations. With Alberta becoming the epicenter, healthcare professionals are urging the public to understand the importance of vaccinations.
Measles Surges in Canada: Unpacking the North American Outbreak

Measles Surges in Canada: Unpacking the North American Outbreak
A deep dive into the measles outbreak ravaging Canada as cases skyrocket, highlighting the role of vaccine hesitancy and community dynamics.
In recent months, Canada has found itself at the forefront of a serious measles outbreak, with over 3,800 infections reported in 2025, predominantly affecting children and infants. This number nearly triples the recorded cases in the United States, despite Canada's smaller population size. Alberta, the hardest-hit province, has recorded the highest per capita measles incidence in North America, prompting public health officials to investigate why the virus is spreading more rapidly in Canada.
The situation is exacerbated by a rise in vaccine hesitancy, which has been intensifying since the COVID-19 pandemic. Notably, there has not been a strong public health figure in Canada comparable to U.S. vaccine skeptics, yet misinformation has permeated communities, particularly among conservative groups like the Low German-speaking Mennonites. This demographic has historically faced vaccination challenges due to cultural beliefs, which have tragically coincided with a surge in anti-vaccine narratives.
According to public health experts, the ongoing outbreak can be traced back to community gatherings, particularly a sizeable Mennonite event where the virus was first seeded. A healthcare provider working near these communities noted that many infections have been identified in unvaccinated individuals, with the outbreak highlighting the critical need for higher vaccination rates.
Research indicates that vaccine uptake has significantly dropped since 2019. In Alberta, for instance, MMR vaccinations decreased nearly 50% in recent years. The hesitance to vaccinate has been compounded by distrust in the healthcare system, fueled by prior experiences of community discrimination and the recent societal turmoil surrounding COVID-19 mandates.
While some public health measures have been implemented to increase vaccinations, such as lowering the age for the measles vaccine in response to the outbreak, the public's response has been tepid compared to prior health emergencies. With Canada having not seen measles represented in such high numbers since 1998, the current outbreak emphasizes an urgent revisitation of public health messaging and community trust.
As families like that of Morgan Birch, whose infant daughter contracted measles, navigate the fallout, there's a growing call for collective responsibility. Birch's concerns echo louder as she advocates for a future where such outbreaks become preventable through adherence to vaccination protocols. The current measles crisis is a stark reminder of the delicate balance between public health and community beliefs, with potential long-term ramifications for health systems nationwide.
The situation is exacerbated by a rise in vaccine hesitancy, which has been intensifying since the COVID-19 pandemic. Notably, there has not been a strong public health figure in Canada comparable to U.S. vaccine skeptics, yet misinformation has permeated communities, particularly among conservative groups like the Low German-speaking Mennonites. This demographic has historically faced vaccination challenges due to cultural beliefs, which have tragically coincided with a surge in anti-vaccine narratives.
According to public health experts, the ongoing outbreak can be traced back to community gatherings, particularly a sizeable Mennonite event where the virus was first seeded. A healthcare provider working near these communities noted that many infections have been identified in unvaccinated individuals, with the outbreak highlighting the critical need for higher vaccination rates.
Research indicates that vaccine uptake has significantly dropped since 2019. In Alberta, for instance, MMR vaccinations decreased nearly 50% in recent years. The hesitance to vaccinate has been compounded by distrust in the healthcare system, fueled by prior experiences of community discrimination and the recent societal turmoil surrounding COVID-19 mandates.
While some public health measures have been implemented to increase vaccinations, such as lowering the age for the measles vaccine in response to the outbreak, the public's response has been tepid compared to prior health emergencies. With Canada having not seen measles represented in such high numbers since 1998, the current outbreak emphasizes an urgent revisitation of public health messaging and community trust.
As families like that of Morgan Birch, whose infant daughter contracted measles, navigate the fallout, there's a growing call for collective responsibility. Birch's concerns echo louder as she advocates for a future where such outbreaks become preventable through adherence to vaccination protocols. The current measles crisis is a stark reminder of the delicate balance between public health and community beliefs, with potential long-term ramifications for health systems nationwide.